A 50% heritability for alcoholism is linked to how one's brain responds to alcohol. Individuals genetically predisposed to feel more stimulated ('fun') from drinking are at higher risk, while those who feel sedated are more protected. The risk is about the positive reinforcement loop, not an innate tolerance.
Related Insights
Counterintuitively, success correlates with higher rates of alcohol problems. High-achievers, often with high negative affect, use alcohol as an effective but destructive tool to manage the intense anxiety and stress that comes with their roles.
The key indicators of a drinking problem are not how much one drinks, but the negative consequences experienced and the inability to control consumption. This framework, focusing on the "three C's" (Consumption, Consequences, Control), redefines problematic drinking away from simple volume metrics.
Humans evolved to have different "drugs of choice" as a survival mechanism. If everyone sought the same rewards, groups would quickly deplete a single resource. This once-adaptive trait now makes us vulnerable to a wide array of modern, hyper-stimulating temptations.
Brain imaging suggests people with ADHD may have a reward pathway that is less activated by stimuli and contains fewer dopamine receptors at baseline. This inherent "reward deficit" could create a state of craving even before exposure to addictive substances, increasing vulnerability.
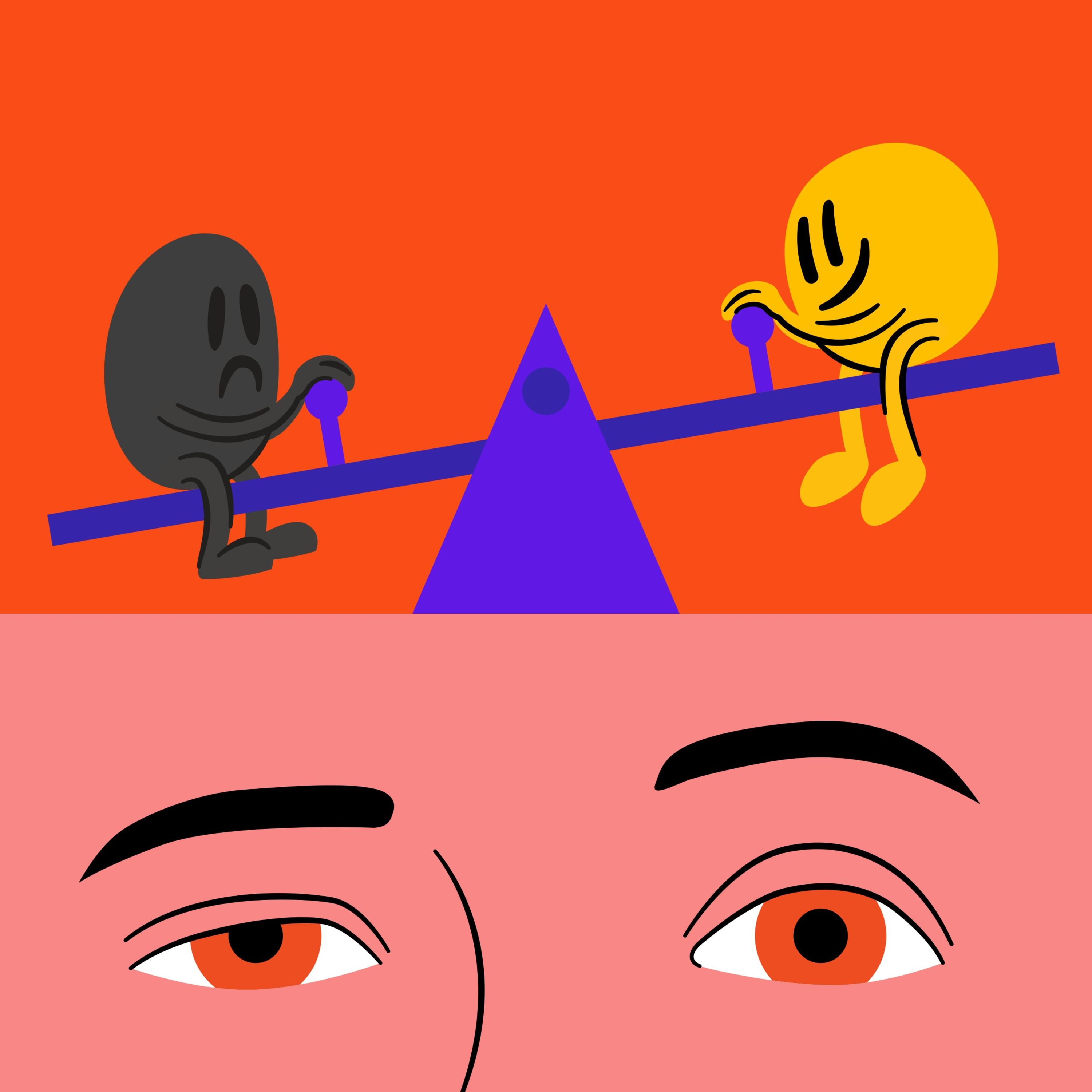
The brain maintains balance by counteracting any deviation to the pleasure side with an equal and opposite reaction to the pain side. This opponent process is why we experience hangovers and why chronic indulgence leads to a dopamine deficit state, driving us to use more just to feel normal.
For millennia, humans consumed weak, fermented beverages in communal settings, providing natural limits. The recent inventions of distillation (high-potency alcohol) and cultural shifts toward private, isolated consumption have removed these biological and social guardrails, making alcohol far more dangerous than it was historically.
Alcohol temporarily reduces anxiety by boosting the neurotransmitter GABA. However, the brain overcompensates by converting GABA into glutamate, an excitatory neurotransmitter. This rebound effect leaves you more anxious than before, creating a self-perpetuating cycle of self-medication.
An animal study shows a rat, when painfully shocked, will immediately try to get cocaine again even after the habit was extinguished. This models how humans under stress revert to high-dopamine rewards because the brain has encoded this as the fastest way out of any painful state.
Addiction isn't defined by the pursuit of pleasure. It's the point at which a behavior, which may have started for rational reasons, hijacks the brain’s reward pathway and becomes compulsive. The defining characteristic is the inability to stop even when the behavior no longer provides pleasure and begins causing negative consequences.
Constantly bombarding our reward pathways causes the brain to permanently weigh down the 'pain' side of its pleasure-pain balance. This alters our baseline mood, or 'hedonic set point,' meaning we eventually need our substance or behavior not to get high, but simply to escape a state of withdrawal and feel normal.