Brain imaging studies show that the brain's reward circuitry (nucleus accumbens) activation in response to drug cues is a more accurate predictor of relapse than the person's own stated commitment to sobriety. This highlights a powerful disconnect between conscious desire and deeply ingrained, subconscious cravings.
Related Insights
Brain imaging suggests people with ADHD may have a reward pathway that is less activated by stimuli and contains fewer dopamine receptors at baseline. This inherent "reward deficit" could create a state of craving even before exposure to addictive substances, increasing vulnerability.
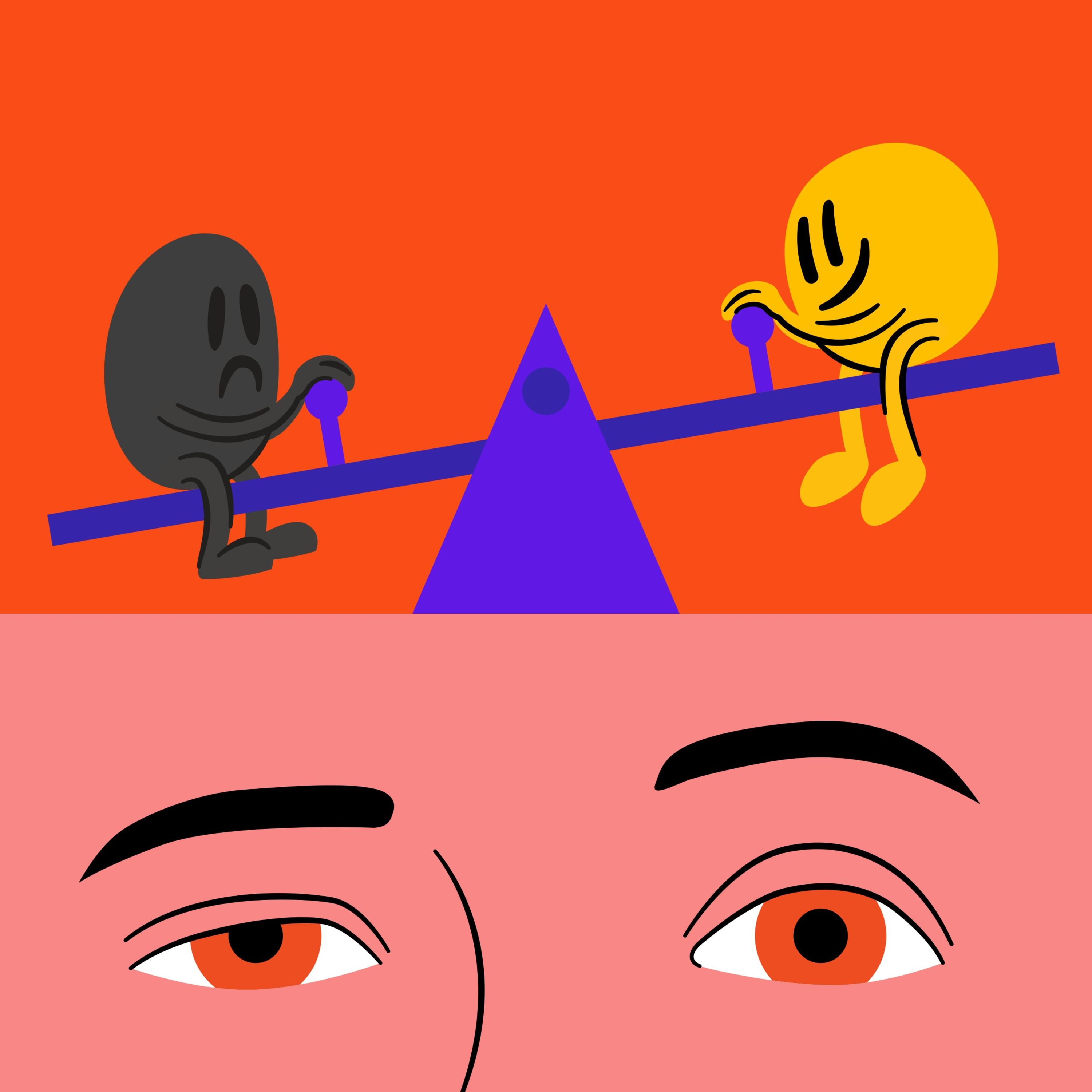
Neuroscience shows pleasure and pain are co-located in the brain and work like a seesaw. When we experience pleasure, the brain immediately compensates by tilting towards pain to restore balance. This neurological 'come down' is why constant pleasure-seeking eventually leads to a state of chronic pain and craving.
According to neuroanatomist Dr. Jill Bolte-Taylor, the brain's left emotional system stores past pain, trauma, and addiction. This isn't a flaw; it's a protective mechanism designed to trigger reactions based on past negative events. Healing involves understanding this system, not erasing it.
To break a bad habit, abstain from your "drug of choice" for at least four weeks. This is the average time needed to escape acute withdrawal (which peaks in the first 14 days) and allow the brain's neuroplasticity to restore its ability to enjoy modest, natural rewards again.
An animal study shows a rat, when painfully shocked, will immediately try to get cocaine again even after the habit was extinguished. This models how humans under stress revert to high-dopamine rewards because the brain has encoded this as the fastest way out of any painful state.
Addiction isn't defined by the pursuit of pleasure. It's the point at which a behavior, which may have started for rational reasons, hijacks the brain’s reward pathway and becomes compulsive. The defining characteristic is the inability to stop even when the behavior no longer provides pleasure and begins causing negative consequences.
Resolving a specific addiction (like alcoholism) doesn't necessarily resolve the underlying genetic or psychological predisposition. This 'diathesis' can re-emerge years later, expressing itself as a new compulsion, such as a sex addiction or compulsive eating, even in someone who has been sober for 20 years.
Constantly bombarding our reward pathways causes the brain to permanently weigh down the 'pain' side of its pleasure-pain balance. This alters our baseline mood, or 'hedonic set point,' meaning we eventually need our substance or behavior not to get high, but simply to escape a state of withdrawal and feel normal.
Willpower is an exhaustible resource. A more effective strategy is "self-binding," where you create literal and metacognitive barriers between yourself and your drug of choice. This friction (e.g., deleting an app) slows you down, giving you the critical time needed to surf a craving without acting on it.
Resolutions often fail because a specific brain network, the "value system," calculates choices based on immediate, vivid rewards rather than distant, abstract benefits. This system heavily discounts the future, meaning the present pleasure of a milkshake will almost always outweigh the vague, far-off goal of better health, creating a constant internal conflict.