Chronic heavy alcohol use causes significant brain damage by accelerating brain atrophy. MRI scans reveal that the brain of a 43-year-old with severe alcohol use disorder can look anatomically similar to the brain of a 90-year-old with dementia, showing a dramatic loss of healthy, active brain tissue.
Related Insights
The key indicators of a drinking problem are not how much one drinks, but the negative consequences experienced and the inability to control consumption. This framework, focusing on the "three C's" (Consumption, Consequences, Control), redefines problematic drinking away from simple volume metrics.
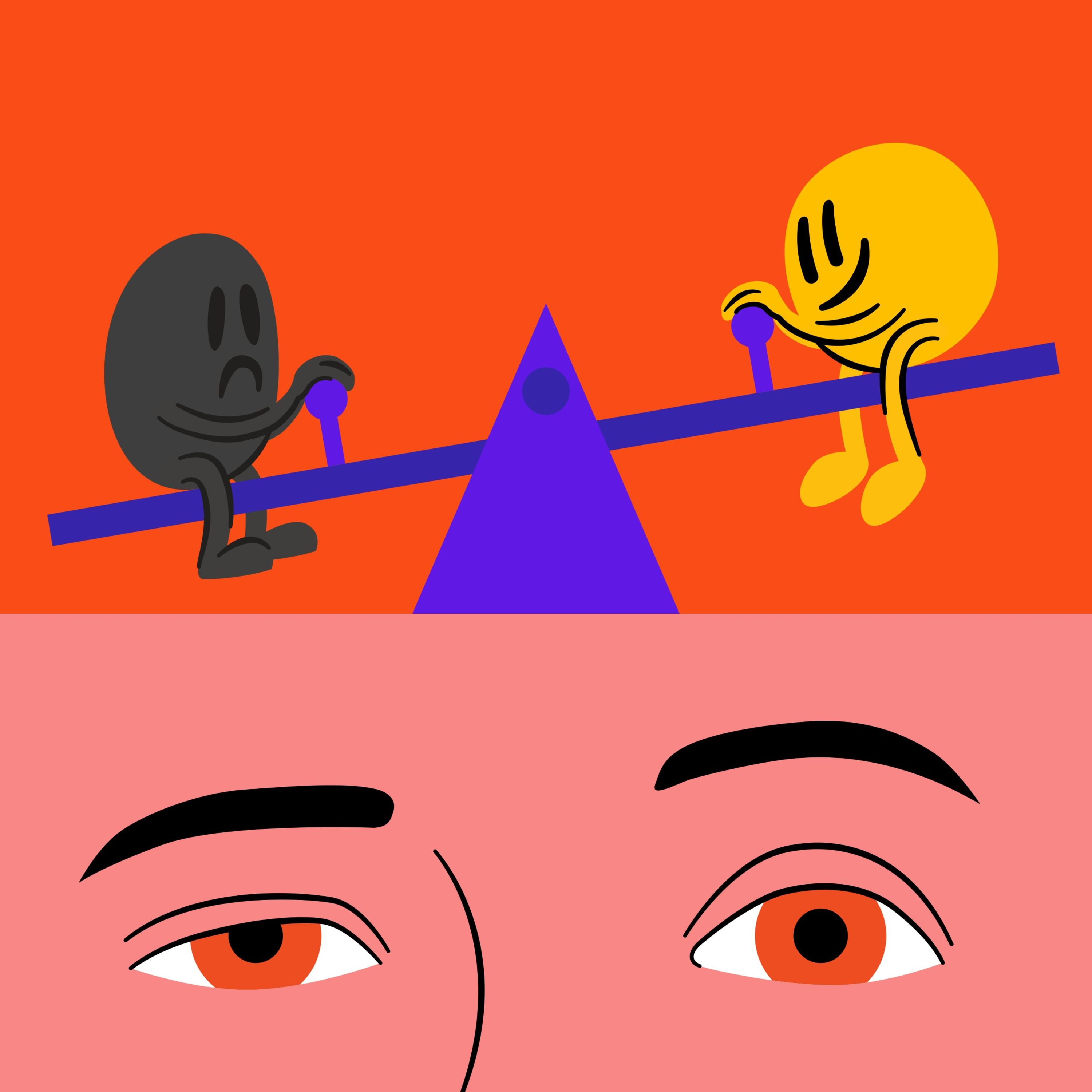
The brain maintains balance by counteracting any deviation to the pleasure side with an equal and opposite reaction to the pain side. This opponent process is why we experience hangovers and why chronic indulgence leads to a dopamine deficit state, driving us to use more just to feel normal.
A subset of people (around 8-10%) are genetically predisposed to feel fewer negative effects from alcohol, like body sway or hangovers. This seeming advantage is a significant risk factor, as they lack the crucial negative feedback signals that tell others to stop drinking, allowing for higher consumption and faster dependency.
For millennia, humans consumed weak, fermented beverages in communal settings, providing natural limits. The recent inventions of distillation (high-potency alcohol) and cultural shifts toward private, isolated consumption have removed these biological and social guardrails, making alcohol far more dangerous than it was historically.
The popular idea that moderate drinking is healthier than abstaining is flawed. Studies creating this 'J-shaped curve' often include former alcoholics with existing health problems in the 'non-drinker' category. This skews the data, making moderate drinkers appear healthier by comparison when, in fact, zero alcohol is best.
Alzheimer's is a disease of midlife. Pathological changes in the brain start to occur from around age 30, but the first noticeable cognitive symptoms typically don't manifest until one's late 60s or 70s. This highlights a crucial, multi-decade window for prevention and intervention.
A 50% heritability for alcoholism is linked to how one's brain responds to alcohol. Individuals genetically predisposed to feel more stimulated ('fun') from drinking are at higher risk, while those who feel sedated are more protected. The risk is about the positive reinforcement loop, not an innate tolerance.
Constantly bombarding our reward pathways causes the brain to permanently weigh down the 'pain' side of its pleasure-pain balance. This alters our baseline mood, or 'hedonic set point,' meaning we eventually need our substance or behavior not to get high, but simply to escape a state of withdrawal and feel normal.
Past studies suggested moderate drinkers were healthier than non-drinkers because the 'non-drinker' control group included people who quit due to existing health problems or prior alcohol damage. When compared to a truly healthy group of very light drinkers, the supposed health benefits of alcohol disappear entirely.
Brain imaging studies show that the brain's reward circuitry (nucleus accumbens) activation in response to drug cues is a more accurate predictor of relapse than the person's own stated commitment to sobriety. This highlights a powerful disconnect between conscious desire and deeply ingrained, subconscious cravings.