While oncologists focus on the low 4% rate of Interstitial Lung Disease (ILD) from neoadjuvant TDXD, surgeons worry this complication could prevent patients from reaching potentially curative surgery, drawing parallels to issues seen with neoadjuvant immunotherapy.
Related Insights
Trastuzumab deruxtecan (TDXD) and datopotamab deruxtecan (Dato-DXd) share the same cytotoxic payload, yet Dato-DXd has a much lower rate of interstitial lung disease (ILD). This indicates the toxicity is driven by the antibody-antigen interaction, not the payload itself.
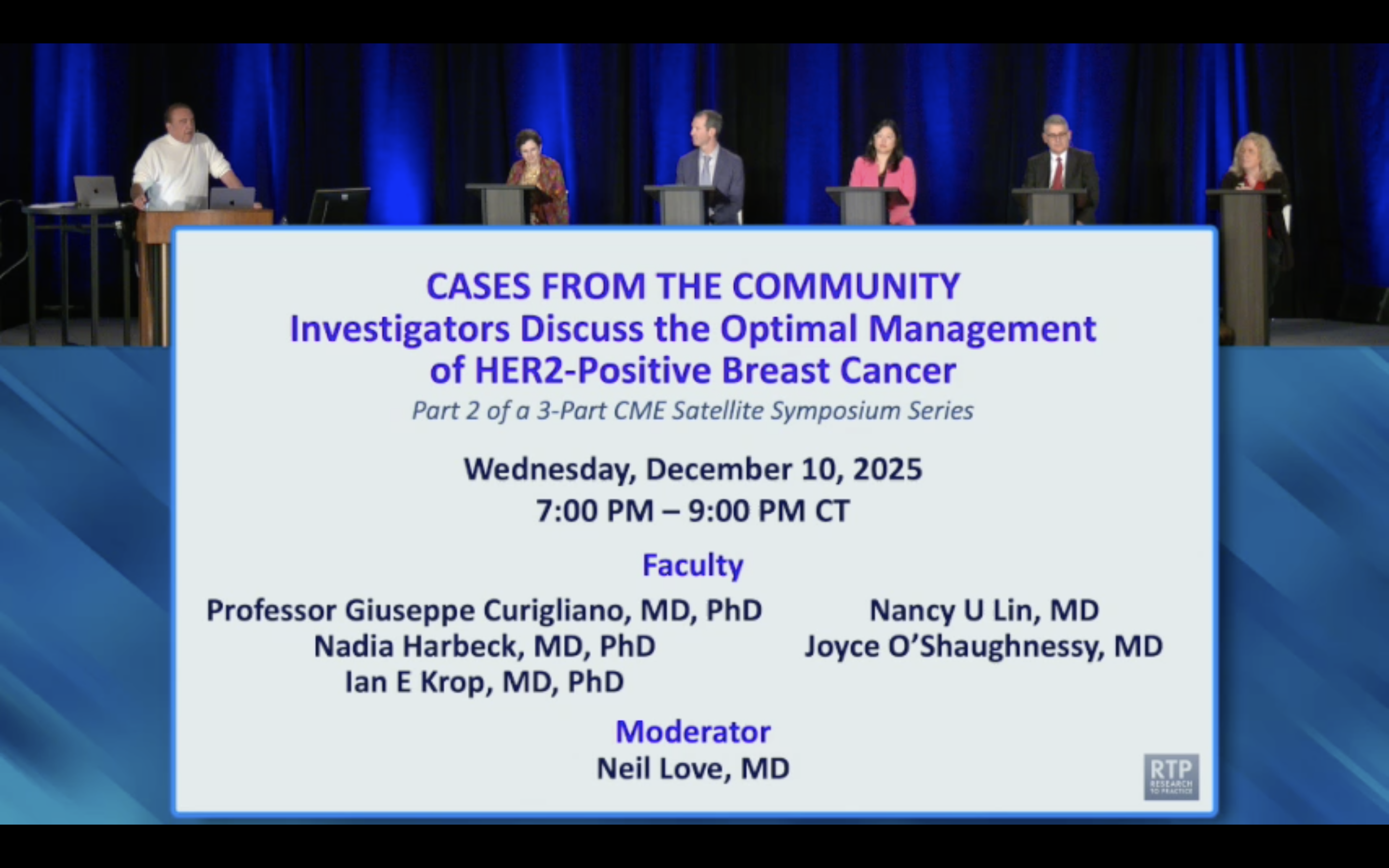
Due to cumulative toxicity concerns with TDXD, particularly ILD, clinicians express more comfort with the shorter 4-cycle neoadjuvant course from DESTINY-Breast11 than the prolonged 14-cycle adjuvant therapy in DESTINY-Breast05, favoring front-loading the treatment.
To manage the risk of interstitial lung disease (ILD) with TDXD, experts now recommend routine screening with high-resolution chest CT scans every 6-12 weeks. This practice aims to catch asymptomatic, grade 1 ILD early, allowing for treatment holds and steroid intervention, which may preserve the option to rechallenge.
When debating immunotherapy risks, clinicians separate manageable side effects from truly life-altering events. Hypothyroidism requiring a daily pill is deemed acceptable, whereas toxicities like diabetes or myocarditis (each ~1% risk) are viewed as major concerns that heavily weigh on the risk-benefit scale for early-stage disease.
While the feared side effect of severe lung inflammation (pneumonitis) did not increase, other immune-mediated adverse events did. This led to higher rates of treatment discontinuation in the experimental arm, potentially negating any benefits of the concurrent approach and contributing to the trial's failure.
Standard cancer surgery often removes lymph nodes—the factories producing immune cells. Administering immunotherapy *before* this destructive process is critical. It arms the immune system while it is still intact and capable of mounting a powerful, targeted response against the tumor.
With highly effective neoadjuvant therapies now available, the surgeon's role in muscle-invasive bladder cancer is evolving. They are moving from being the primary decider and treater to being a key manager of a 'perioperative bundle,' where their first goal is often to get patients to medical oncology for systemic treatment.
The KIDO 905 trial revealed high rates of adverse events even in the control arm receiving only surgery. This suggests the invasive procedure itself is a major source of patient harm, paving the way for future surgery-free regimens if systemic treatments like EVP prove sufficiently effective.
Dr. Radvanyi advocates for a paradigm shift: treating almost all cancers with neoadjuvant immunotherapy immediately after diagnosis. This "kickstarts" an immune response before standard treatments like surgery and chemotherapy, which are known to be immunosuppressive, can weaken the patient's natural defenses against the tumor.
For N2+ EGFR-mutant NSCLC, clinicians now face a choice. Combining neoadjuvant osimertinib with chemotherapy is potent and gets treatment done upfront, but osimertinib monotherapy is better tolerated, reducing the risk of toxicity that could prevent a patient from reaching their planned surgery.