Cancers with estrogen receptor (ER) expression of 50% or less, while technically HR+, often behave biologically like basal or triple-negative tumors. These cancers are not primarily endocrine-driven and show a significant benefit from the addition of immune checkpoint inhibitors, challenging traditional subtype classifications.
Related Insights
The drug exhibits a multimodal mechanism. It not only reverses chemoresistance and halts tumor growth but also 'turns cold tumors hot' by forcing cancer cells to display markers that make them visible to the immune system. This dual action of direct attack and immune activation creates a powerful synergistic effect.
An innovative strategy for solid tumors involves using bispecific T-cell engagers to target the tumor stroma—the protective fibrotic tissue surrounding the tumor. This novel approach aims to first eliminate this physical barrier, making the cancer cells themselves more vulnerable to subsequent immune attack.
NGS testing is revealing that acquired HER2 kinase domain mutations, not amplifications, are an emerging resistance mechanism in ER+ lobular breast cancer. This creates a targetable population for HER2 TKIs like neratinib or tucatinib, offering a new line of targeted therapy.
A leading hypothesis for why adding immunotherapy to chemoradiation failed is that radiation, particularly for central tumors, destroys the very lymphocytes immunotherapy aims to activate. This biological mechanism suggests the radiation essentially canceled out the drug's intended effect.
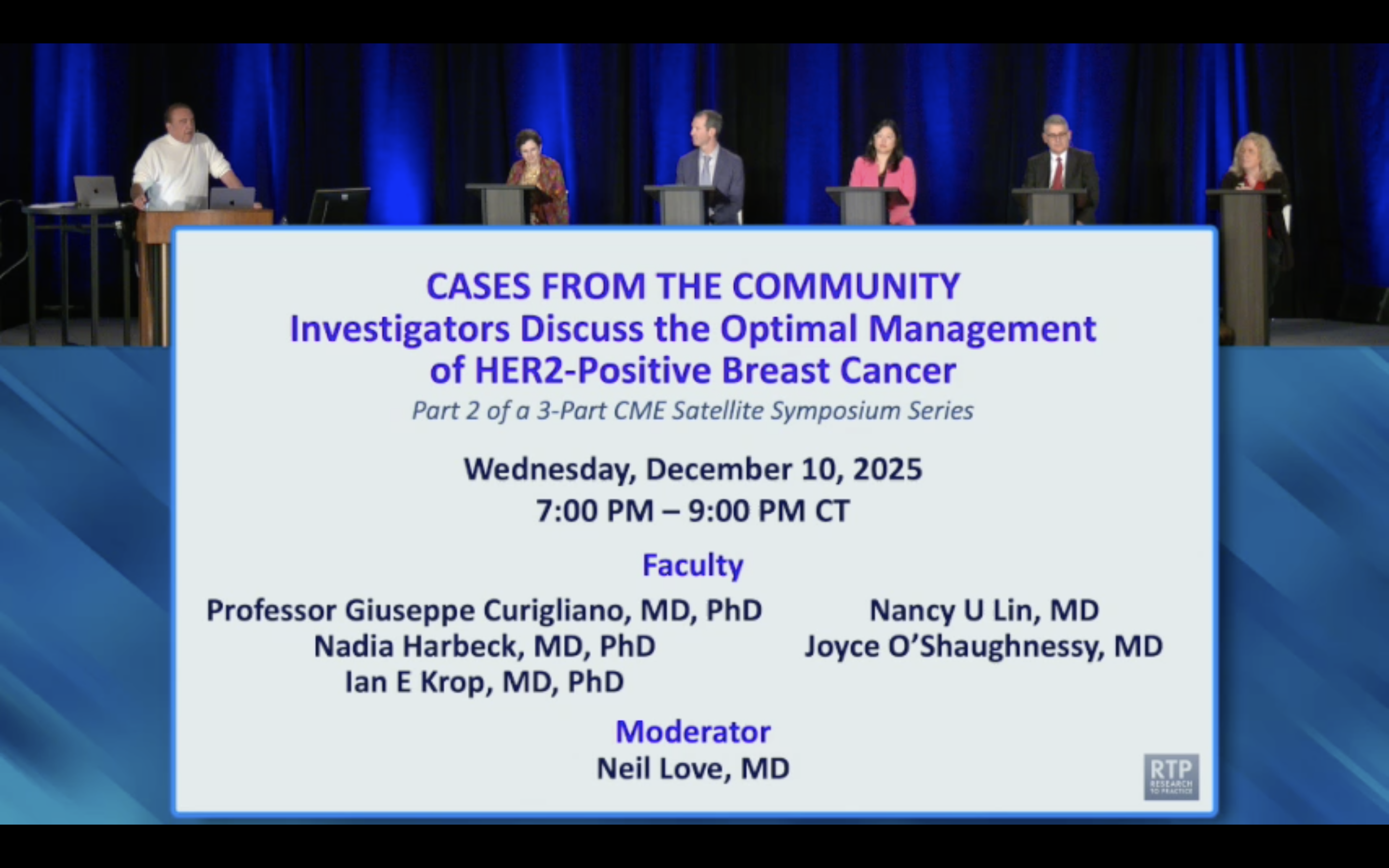
The DESTINY-Breast11 trial showed a neoadjuvant regimen of TDXD followed by THP achieved a 67.3% pathologic complete response (pCR) rate in high-risk HER2+ breast cancer. This is the highest pCR rate seen in a registrational trial, signaling a potential new standard of care.
A subset of breast cancers (10-15%) are "non-shedders," meaning they don't release detectable ctDNA. Patients with these tumors have excellent outcomes regardless of chemotherapy, suggesting that surgery alone might be a sufficient and less toxic treatment for this specific group.
Successful immunotherapies like anti-PD-1 work by shifting the battlefield's arithmetic. They enhance the efficiency of each T-cell, allowing one cell to destroy five or ten cancer cells instead of three. This turns the fight into a 'numbers game' that the immune system can finally win.
Developers often test novel agents in late-line settings because the control arm is weaker, increasing the statistical chance of success. However, this strategy may doom effective immunotherapies by testing them in biologically hostile, resistant tumors, masking their true potential.
To combat immunosuppressive "cold" tumors, new trispecific antibodies are emerging. Unlike standard T-cell engagers that only provide the primary CD3 activation signal, these drugs also deliver the crucial co-stimulatory signal (e.g., via CD28), ensuring full T-cell activation in microenvironments where this second signal is naturally absent.
Immunotherapies can be effective even without causing significant tumor shrinkage. Immunocore's drug KimTrack had a low 5-7% objective response rate (ORR) but demonstrated a massive overall survival (OS) benefit, challenging the reliance on traditional chemotherapy metrics for evaluating modern cancer treatments.