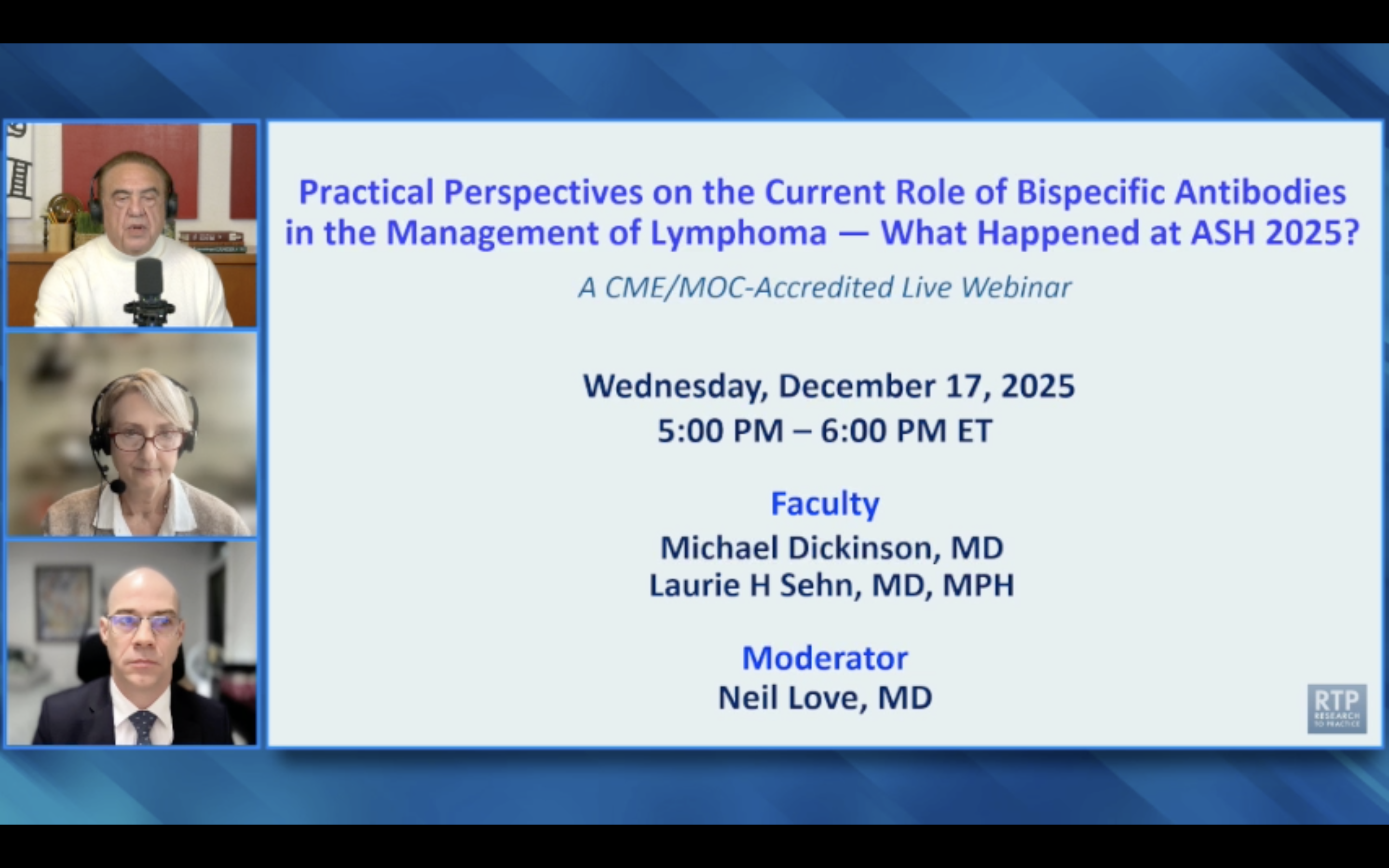
Emerging data reveals significant synergy when combining antibody-drug conjugates (ADCs) like polatuzumab vedotin with bispecific antibodies like glofitumab. These combinations show impressive results in relapsed/refractory non-Hodgkin lymphoma, signaling a major future direction for developing more potent therapies.
Related Insights
The future of advanced prostate cancer treatment may involve combining ADCs with bispecific T-cell engagers. This strategy could use ADCs for a short duration to deliver a potent hit, followed by immunotherapy to achieve durable remission, potentially reducing toxicity and enabling earlier use.
Combining polatuzumab vedotin with bispecific antibodies appears particularly effective for patients with double-hit lymphoma. This is significant because these high-risk patients, who have poor prognoses, were notably excluded from pivotal trials like STAR GLOW, suggesting a potential new standard for this specific subgroup.
The rationale for developing Sigvotatug Vedotin extends beyond its direct cytotoxic effect. Preclinical data shows that blocking the IB6 pathway can increase the potency of PD-1/PD-L1 checkpoint inhibitors, suggesting a powerful synergistic effect that could lead to highly effective future combination therapies.
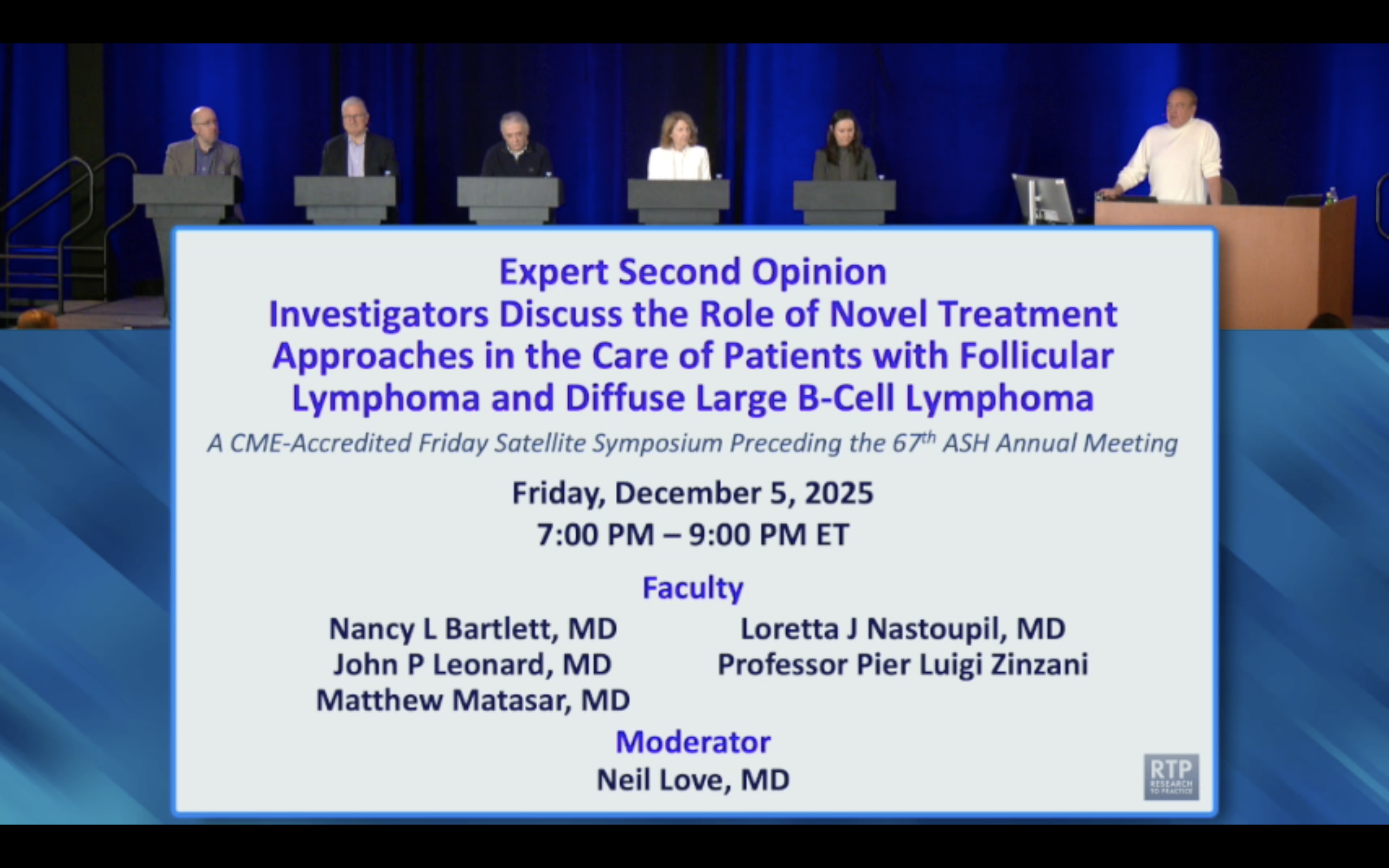
In follicular lymphoma, the treatment goal is durable remission with manageable toxicity, not necessarily a cure. Therefore, clinicians frequently prefer using a bispecific antibody first, reserving the more complex and toxic CAR-T cell therapy for transformed disease or after a bispecific fails.
Not all CD20-targeting bispecifics can be combined with rituximab. Mosunetuzumab binds the same epitope, causing competition. However, glofitamab and epcoritamab bind different epitopes, allowing for logical and potentially synergistic combinations with rituximab-based regimens.
Pathways like integrins have long been of interest but lacked effective therapeutic approaches. The advent of new technologies, such as antibody-drug conjugates and checkpoint inhibitors, has created opportunities to re-explore these older targets with potent, modern drugs, breathing new life into decades-old research.
Unlike older antibody-drug conjugates (ADCs), newer agents are designed so their chemotherapy payload can diffuse out of the target cell and kill nearby tumor cells that may not even express the target antigen. This "bystander effect" significantly enhances their anti-tumor activity.
While immunotherapy was a massive leap forward, Dr. Saav Solanki states the next innovation frontier is combining it with newer modalities. Antibody-drug conjugates (ADCs) and T-cell engagers are being used to recruit the immune system into the tumor microenvironment, helping patients who don't respond to current immunotherapies.
The dramatic efficacy boost from adding epcoritamab suggests it's the primary driver of patient benefit, not just an adjunct. This shifts the conceptual framework, positioning the bispecific antibody as the new therapeutic backbone, with rituximab and lenalidomide as supportive agents.
The ECHELON-3 trial showed that brentuximab vedotin plus R-squared is effective in relapsed/refractory DLBCL, even in patients with negligible CD30 expression. This suggests the drug's benefit may stem from immune synergy or other mechanisms, not just direct CD30 targeting.