While eradicating H. pylori can improve platelet counts in ITP, its efficacy shows significant geographical variation. The strategy is successful in Europe and Japan but often fails in the United States, a difference attributed to regional variations in H. pylori strains.
Related Insights
The target platelet count for ITP patients should be tailored to their lifestyle, bleeding history, and quality of life goals. A normal platelet count is not necessary, and different thresholds are appropriate for different patients (e.g., someone planning a ski trip versus a sedentary individual).
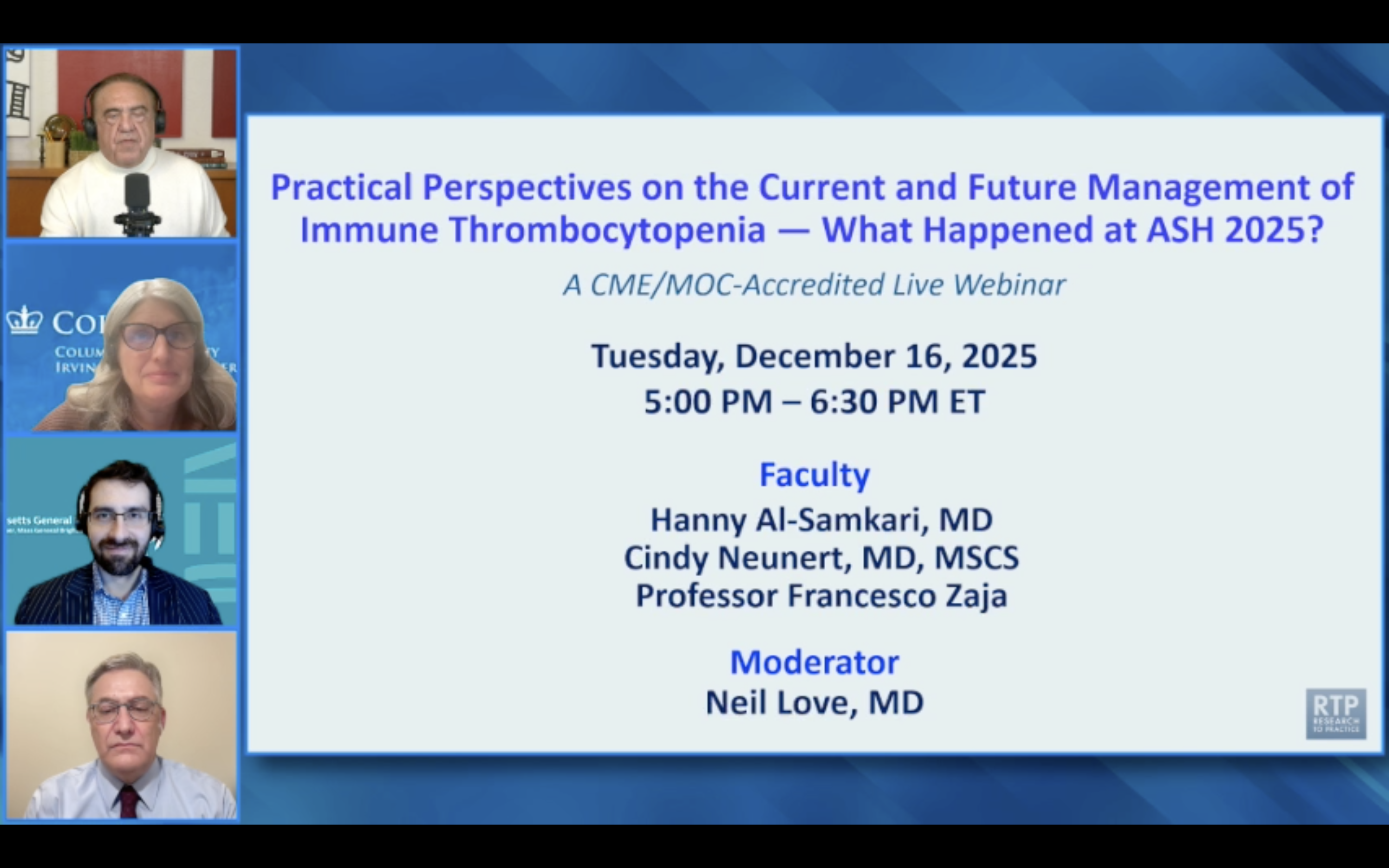
ITP caused by immune checkpoint inhibitors (ICIs) is rare (0.25% incidence) but generally has a good prognosis. Most patients respond to standard first-line ITP therapies, and approximately 70% of those re-challenged with the ICI can continue treatment without a recurrence of ITP.
Beyond raising platelet counts, the newly approved BTK inhibitor rilzabrutinib provides dramatic improvements in the fatigue associated with ITP. This unique benefit, likely due to its anti-inflammatory properties, makes it a strong consideration for patients where fatigue is a primary quality of life issue.
The gut microbiome exists in a stable state with a resilience that makes it difficult to alter permanently. After short-term disruptions like antibiotics or diet changes, it often 'snaps back' to its original composition. This means meaningful, long-term change requires sustained effort to establish a new, stable microbial state rather than temporary interventions.
Patients with ITP who fail or are intolerant to one TPO receptor agonist (e.g., eltrombopag) should not be considered a class failure. Switching to another TPO agent is a viable strategy that can induce a response in nearly half of these cases, particularly for intolerance.
Evolutionary modeling shows that taking antibiotics beyond symptom resolution can be counterproductive. It needlessly kills off susceptible bacteria, creating a perfect environment for resistant strains to flourish. The optimal strategy is often to stop once the immune system can handle the rest, contrary to decades of medical advice.
Studies of traditional populations show their microbiomes are vastly different from those in industrialized nations. This suggests that what is considered a 'healthy' American microbiome might actually be a perturbed state, silently predisposing individuals to chronic inflammatory and metabolic diseases due to factors like antibiotics and diet.
Unlike in Europe, US farmers often spray wheat with glyphosate (Roundup) to accelerate drying before harvest. This chemical is known to disrupt the gut microbiome by killing beneficial bacteria. This practice could explain why some Americans experience digestive distress from domestic wheat but can eat pasta in Italy without issue.
Historical data showing high cure rates for splenectomy in ITP is outdated. Recent data indicates that if a patient has already failed both a TPORA and rituximab, the chance of a successful splenectomy is less than 50%, repositioning it as a later-line salvage option.
In cases of severe ITP unresponsive to standard therapies, the anti-CD38 monoclonal antibody daratumumab can be highly effective. It works by eliminating the long-lived plasma cells responsible for secreting platelet autoantibodies, a mechanism distinct from other ITP treatments.