Apply financial forecasting techniques to large patient databases. By treating individual patient data points like historical stock prices, researchers can build complex regression models to project future health outcomes, an innovative approach that earns recognition from national medical academies.
Related Insights
Beyond early discovery, LLMs deliver significant value in clinical trials. They accelerate timelines by automating months of post-trial documentation work. More strategically, they can improve trial success rates by analyzing genomic data to identify patient populations with a higher likelihood of responding to a treatment.
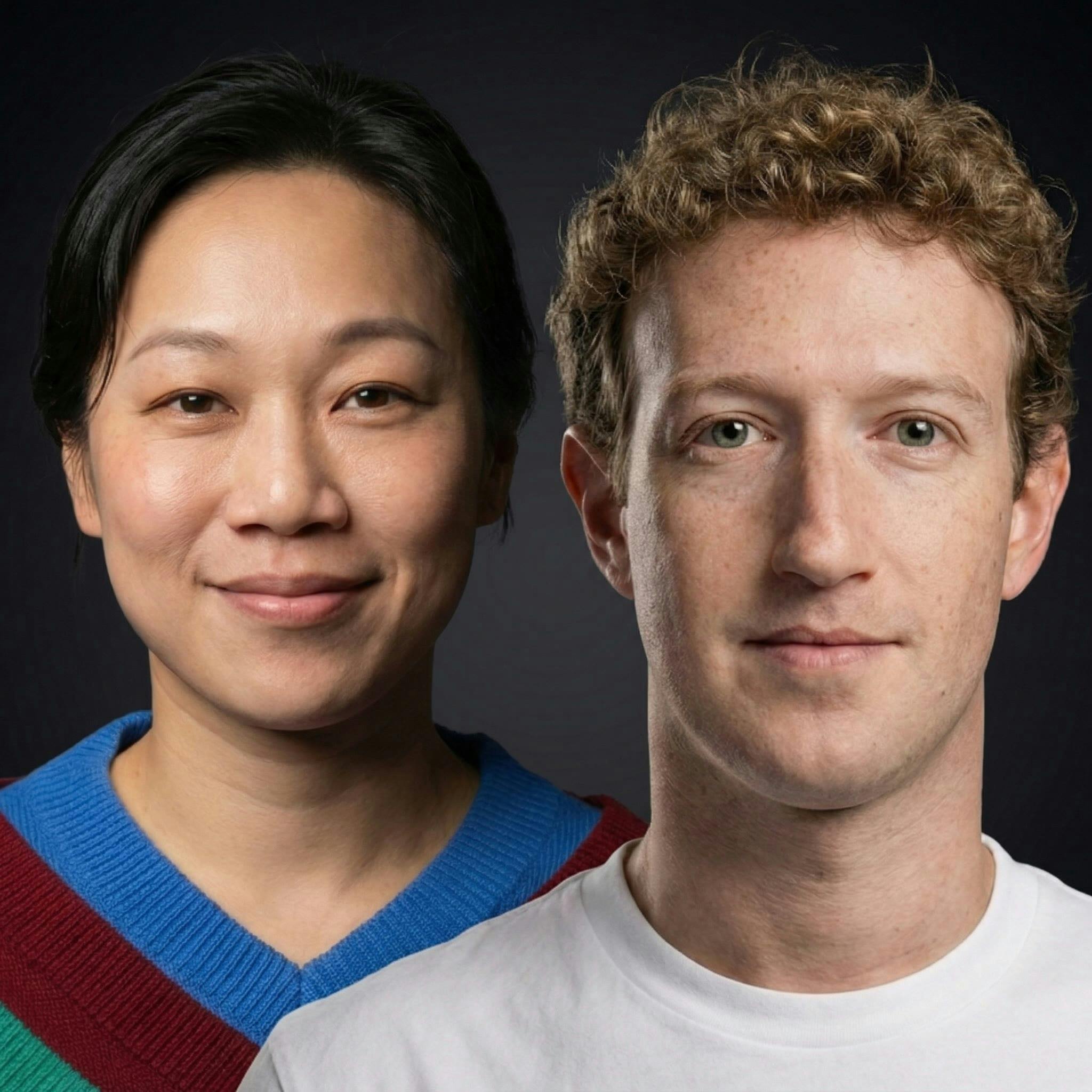
The endgame for CZI's work is hyper-personalized, "N of one" medicine. Instead of the current empirical approach (e.g., trying different antidepressants for months), AI models will simulate an individual's unique biology to predict which specific therapy will work, eliminating guesswork and patient suffering.
AI's most significant impact won't be on broad population health management, but as a diagnostic and decision-support assistant for physicians. By analyzing an individual patient's risks and co-morbidities, AI can empower doctors to make better, earlier diagnoses, addressing the core problem of physicians lacking time for deep patient analysis.
The traditional drug-centric trial model is failing. The next evolution is trials designed to validate the *decision-making process* itself, using platforms to assign the best therapy to heterogeneous patient groups, rather than testing one drug on a narrow population.
As AI enables early disease prediction (like Grail's cancer test), the number of sick patients will decrease. This erodes the traditional drug sales model, forcing pharma companies to create new revenue streams by monetizing predictive data and insights.
By analyzing real-world data with machine learning, Walgreens can identify patients at risk of non-adherence before a clinical issue arises. This allows for early, personalized interventions, moving beyond simply reacting to missed doses or therapy drop-offs.
The progress of AI in predicting cancer treatment is stalled not by algorithms, but by the data used to train them. Relying solely on static genetic data is insufficient. The critical missing piece is functional, contextual data showing how patient cells actually respond to drugs.
The next frontier in preclinical research involves feeding multi-omics and spatial data from complex 3D cell models into AI algorithms. This synergy will enable a crucial shift from merely observing biological phenomena to accurately predicting therapeutic outcomes and patient responses.
The low-hanging fruit of finding a single predictive biomarker is gone. The next frontier for bioinformatics is developing complex, 'multimodal models' that integrate several data points to predict outcomes. The key challenge is creating sophisticated models that still yield practical, broadly applicable clinical insights.
A major frustration in genetics is finding 'variants of unknown significance' (VUS)—genetic anomalies with no known effect. AI models promise to simulate the impact of these unique variants on cellular function, moving medicine from reactive diagnostics to truly personalized, predictive health.