The bispecific antibody zanidatumab causes HER2 receptors to cluster into "caps." This unique structure activates complement-dependent cytotoxicity (CDC), a potent immune response not achievable with older HER2 agents like trastuzumab, explaining its enhanced clinical activity.
Related Insights
The drug exhibits a multimodal mechanism. It not only reverses chemoresistance and halts tumor growth but also 'turns cold tumors hot' by forcing cancer cells to display markers that make them visible to the immune system. This dual action of direct attack and immune activation creates a powerful synergistic effect.
Unlike T-cell engaging therapies, the bispecific antibody zanidatumab does not cause cytokine release syndrome (CRS). This unique safety feature is because it binds to two distinct sites on the HER2 receptor itself, rather than engaging T-cells, providing a key toxicity advantage.
An innovative strategy for solid tumors involves using bispecific T-cell engagers to target the tumor stroma—the protective fibrotic tissue surrounding the tumor. This novel approach aims to first eliminate this physical barrier, making the cancer cells themselves more vulnerable to subsequent immune attack.
Successful immunotherapies like anti-PD-1 work by shifting the battlefield's arithmetic. They enhance the efficiency of each T-cell, allowing one cell to destroy five or ten cancer cells instead of three. This turns the fight into a 'numbers game' that the immune system can finally win.
Accession's second product is a bispecific antibody that binds to all cancer cells. While this would be dangerously toxic if delivered systemically, their targeted virus delivery system ensures it is only produced inside the tumor. This strategy makes previously "undruggable" therapeutic concepts viable.
To combat immunosuppressive "cold" tumors, new trispecific antibodies are emerging. Unlike standard T-cell engagers that only provide the primary CD3 activation signal, these drugs also deliver the crucial co-stimulatory signal (e.g., via CD28), ensuring full T-cell activation in microenvironments where this second signal is naturally absent.
While immunotherapy was a massive leap forward, Dr. Saav Solanki states the next innovation frontier is combining it with newer modalities. Antibody-drug conjugates (ADCs) and T-cell engagers are being used to recruit the immune system into the tumor microenvironment, helping patients who don't respond to current immunotherapies.
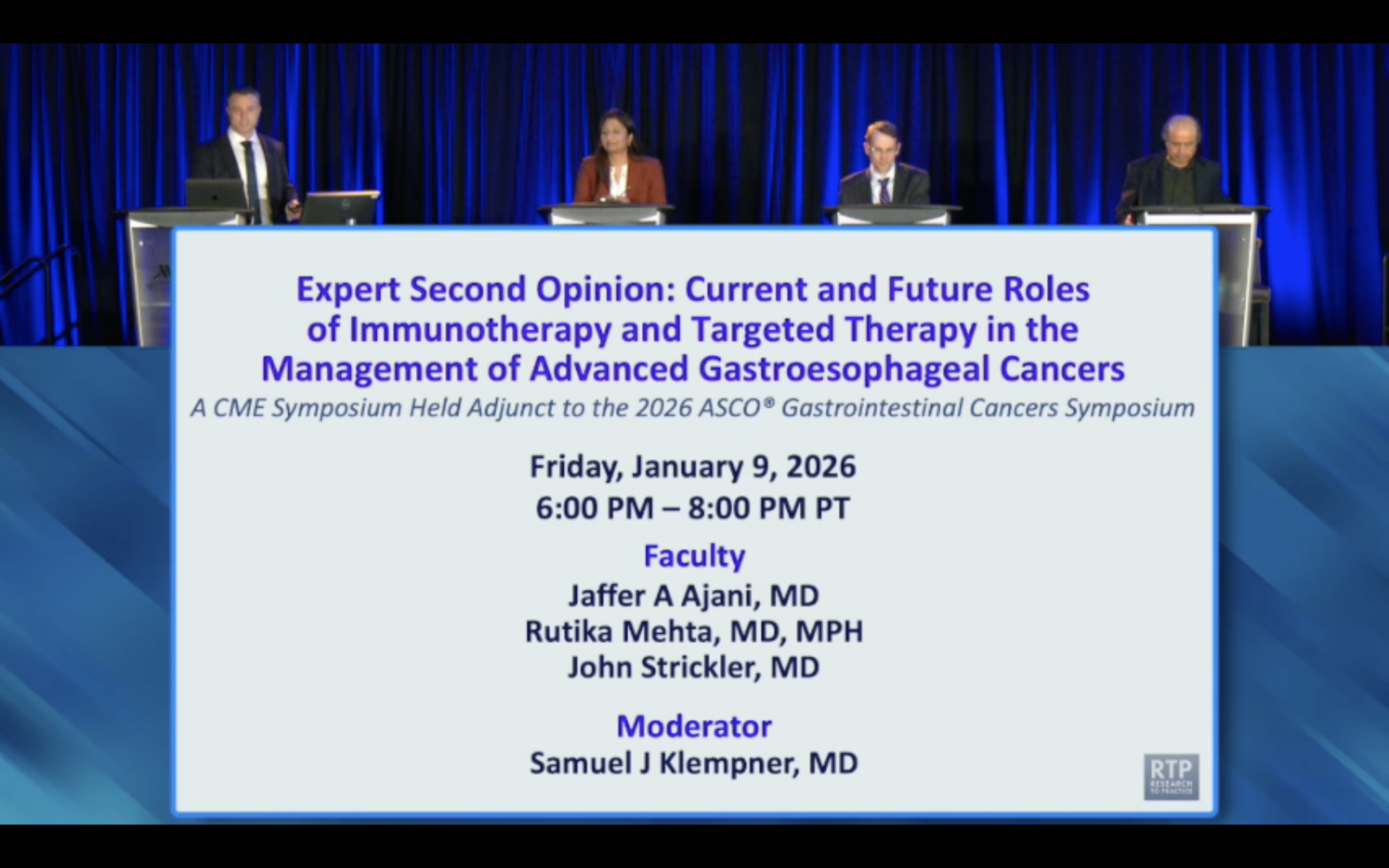
Contrary to concerns about cross-resistance between HER2 antibody-drug conjugates (ADCs), retrospective data shows TDM-1 remains effective after progression on TDXD. This suggests the different cytotoxic payloads are key, allowing for effective sequencing and challenging the assumption that progression on one ADC class member precludes using another.
Emerging data reveals significant synergy when combining antibody-drug conjugates (ADCs) like polatuzumab vedotin with bispecific antibodies like glofitumab. These combinations show impressive results in relapsed/refractory non-Hodgkin lymphoma, signaling a major future direction for developing more potent therapies.
Bi-specific T-cell engagers (BiTEs) are highly immunogenic because the mechanism activating T-cells to kill cancer also primes them to mount an immune response against the drug itself. This 'collateral effect' is an inherent design challenge for this drug class.