Frontline treatment selection hinges on histology. Non-epithelioid mesothelioma responds poorly to chemotherapy, making dual immunotherapy (Nivo/Ipi) the clear choice. For epithelioid cases, chemo-immunotherapy is a strong option, especially for symptomatic patients, due to its higher and faster response rate.
Related Insights
Contrary to its role in lung cancer, PD-L1 expression does not predict benefit from immunotherapy in mesothelioma. Data from major trials shows similar outcomes regardless of PD-L1 status, leading clinicians to omit this test entirely and streamline treatment decisions.
The failure of the concurrent chemo-immuno-radiation approach has not stalled progress. Instead, new clinical trials are actively exploring novel strategies like SBRT boosts, dual checkpoint inhibitors, radiosensitizing nanoparticles, and induction immunotherapy to improve upon the current standard of care.
Data from the Checkmate 743 trial shows that patients who stopped dual immunotherapy (Nivo/Ipi) due to toxicity can still achieve long-term benefits. A third of these patients had an ongoing response at three years, despite stopping treatment after only four months on average, providing confidence in the regimen.
While the feared side effect of severe lung inflammation (pneumonitis) did not increase, other immune-mediated adverse events did. This led to higher rates of treatment discontinuation in the experimental arm, potentially negating any benefits of the concurrent approach and contributing to the trial's failure.
The future of GYN oncology immunotherapy is diverging. For responsive cancers like endometrial, the focus is on refining biomarkers and overcoming resistance. For historically resistant cancers like ovarian, the strategy shifts to using combinatorial approaches (e.g., CAR-NKs, vaccines) to fundamentally alter the tumor microenvironment itself, making it more receptive to an immune response.
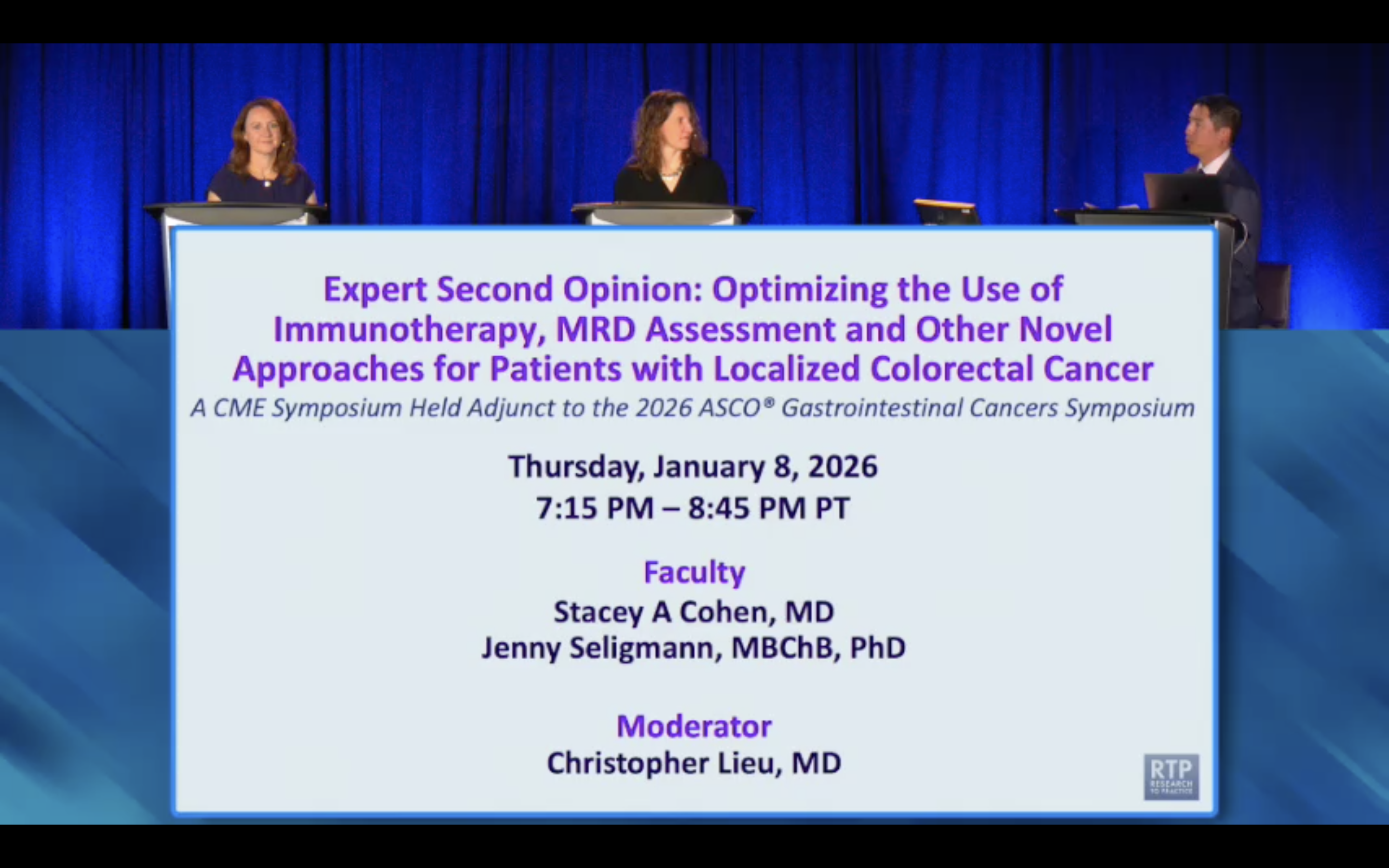
While the ATOMIC trial established FOLFOX plus atezolizumab as a new standard for adjuvant therapy in MSI-high colon cancer, its design lacked an immunotherapy-only arm. This leaves a critical, unanswered question about the actual contribution and necessity of the chemotherapy component.
The next frontier in CSCC isn't just about new drugs, but about optimizing existing ones. A key research area is determining the minimum number of immunotherapy doses required for an optimal response—potentially just one or two—to limit toxicity, reduce treatment burden, and personalize care for high-risk patients.
Standard cancer surgery often removes lymph nodes—the factories producing immune cells. Administering immunotherapy *before* this destructive process is critical. It arms the immune system while it is still intact and capable of mounting a powerful, targeted response against the tumor.
For patients with very high-burden or symptomatic mesothelioma, clinicians may deviate from standard guidelines. They may choose chemo-immunotherapy to maximize the chance of a rapid response, viewing it as their single best opportunity to control the disease, especially if the patient's condition is precarious.
Dr. Radvanyi advocates for a paradigm shift: treating almost all cancers with neoadjuvant immunotherapy immediately after diagnosis. This "kickstarts" an immune response before standard treatments like surgery and chemotherapy, which are known to be immunosuppressive, can weaken the patient's natural defenses against the tumor.