The regimen's profound success in relapsed/refractory patients is not an endpoint, but a launchpad. It provides the rationale for the ongoing Epcor FL2 trial, which directly challenges standard chemoimmunotherapy and could establish a chemotherapy-free, bispecific-based combination as the new first-line standard of care.
Related Insights
The future of advanced prostate cancer treatment may involve combining ADCs with bispecific T-cell engagers. This strategy could use ADCs for a short duration to deliver a potent hit, followed by immunotherapy to achieve durable remission, potentially reducing toxicity and enabling earlier use.
Corvus Pharmaceuticals is already planning frontline combination trials for its T-cell lymphoma drug. The drug's favorable safety profile is the critical enabler, allowing it to be paired with chemotherapy and used as a long-term maintenance therapy to prolong remissions—a strategy unavailable to more toxic drugs.
A modified three-step-up dosing schedule for epcoritamab drastically reduced cytokine release syndrome (CRS) rates to 26%, with no severe events. This safety profile supports fully outpatient administration, making this highly effective regimen accessible to community practices without immediate hospital access.
The failure of the concurrent chemo-immuno-radiation approach has not stalled progress. Instead, new clinical trials are actively exploring novel strategies like SBRT boosts, dual checkpoint inhibitors, radiosensitizing nanoparticles, and induction immunotherapy to improve upon the current standard of care.
An innovative strategy for solid tumors involves using bispecific T-cell engagers to target the tumor stroma—the protective fibrotic tissue surrounding the tumor. This novel approach aims to first eliminate this physical barrier, making the cancer cells themselves more vulnerable to subsequent immune attack.
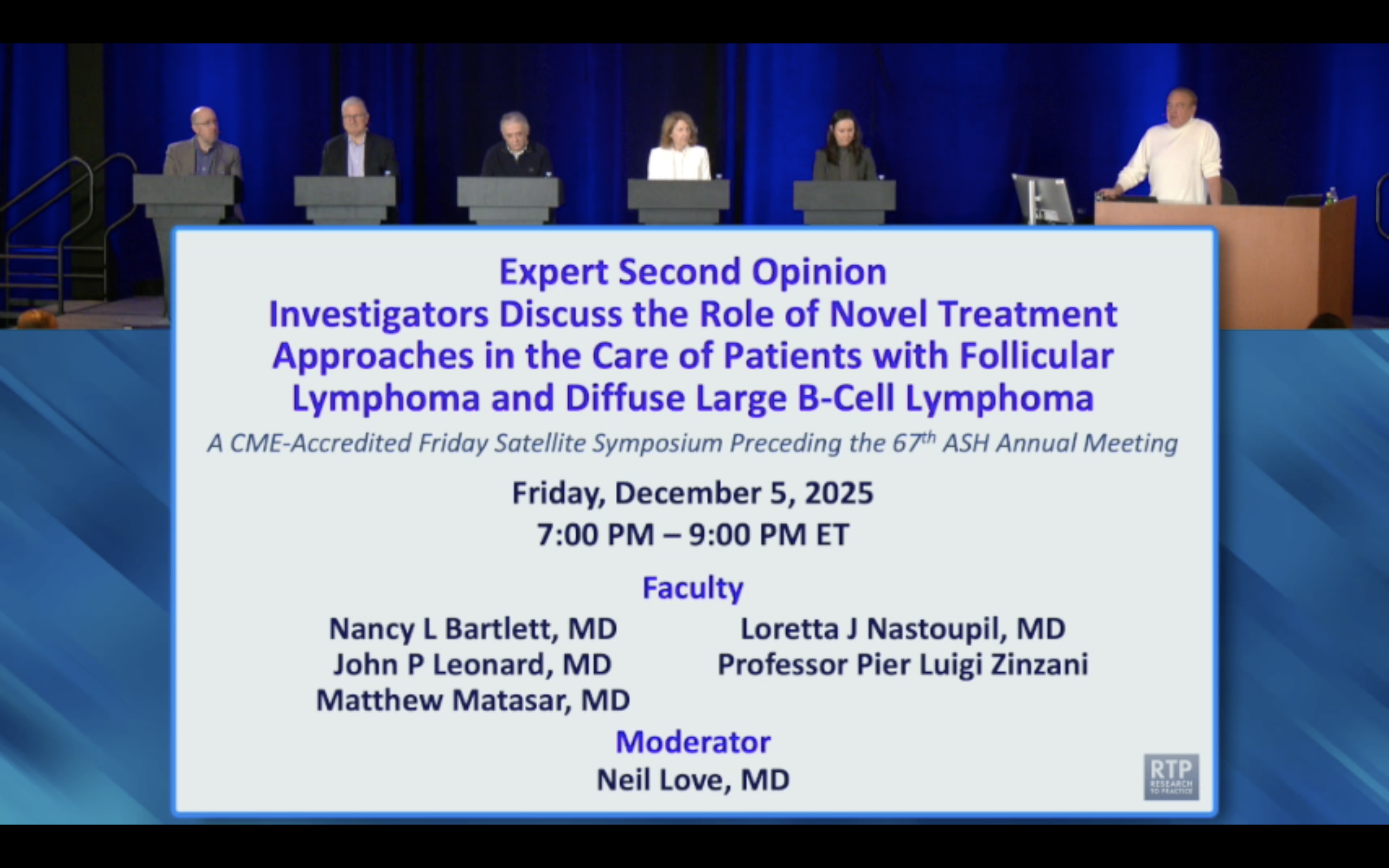
Beyond approving the triplet combination, the positive Epcor FL1 trial data had a significant ripple effect. It solidified the drug's overall profile, leading to the conversion of its prior provisional (accelerated) approvals for monotherapy in follicular lymphoma and DLBCL into full, traditional approvals.
An expert argues the path to curing metastatic cancer may mirror pediatric ALL's history: combining all highly active drugs upfront. Instead of sequencing treatments after failure, the focus should be on powerful initial regimens that eradicate cancer, even if it means higher initial toxicity.
Not all CD20-targeting bispecifics can be combined with rituximab. Mosunetuzumab binds the same epitope, causing competition. However, glofitamab and epcoritamab bind different epitopes, allowing for logical and potentially synergistic combinations with rituximab-based regimens.
Actuate employed a master protocol that tested their drug alongside eight different standard-of-care chemotherapies in patients who had already failed them. This design efficiently demonstrated the drug's ability to reverse chemo-resistance across multiple histologies, informing their Phase 2 strategy.
The dramatic efficacy boost from adding epcoritamab suggests it's the primary driver of patient benefit, not just an adjunct. This shifts the conceptual framework, positioning the bispecific antibody as the new therapeutic backbone, with rituximab and lenalidomide as supportive agents.