While AI is on the verge of cracking preclinical challenges, the biggest problem is the high drug failure rate in human trials. The next wave of innovation will use AI to design molecules for properties that predict human efficacy, addressing the fundamental reason drugs fail late-stage.
Related Insights
AI modeling transforms drug development from a numbers game of screening millions of compounds to an engineering discipline. Researchers can model molecular systems upfront, understand key parameters, and design solutions for a specific problem, turning a costly screening process into a rapid, targeted design cycle.
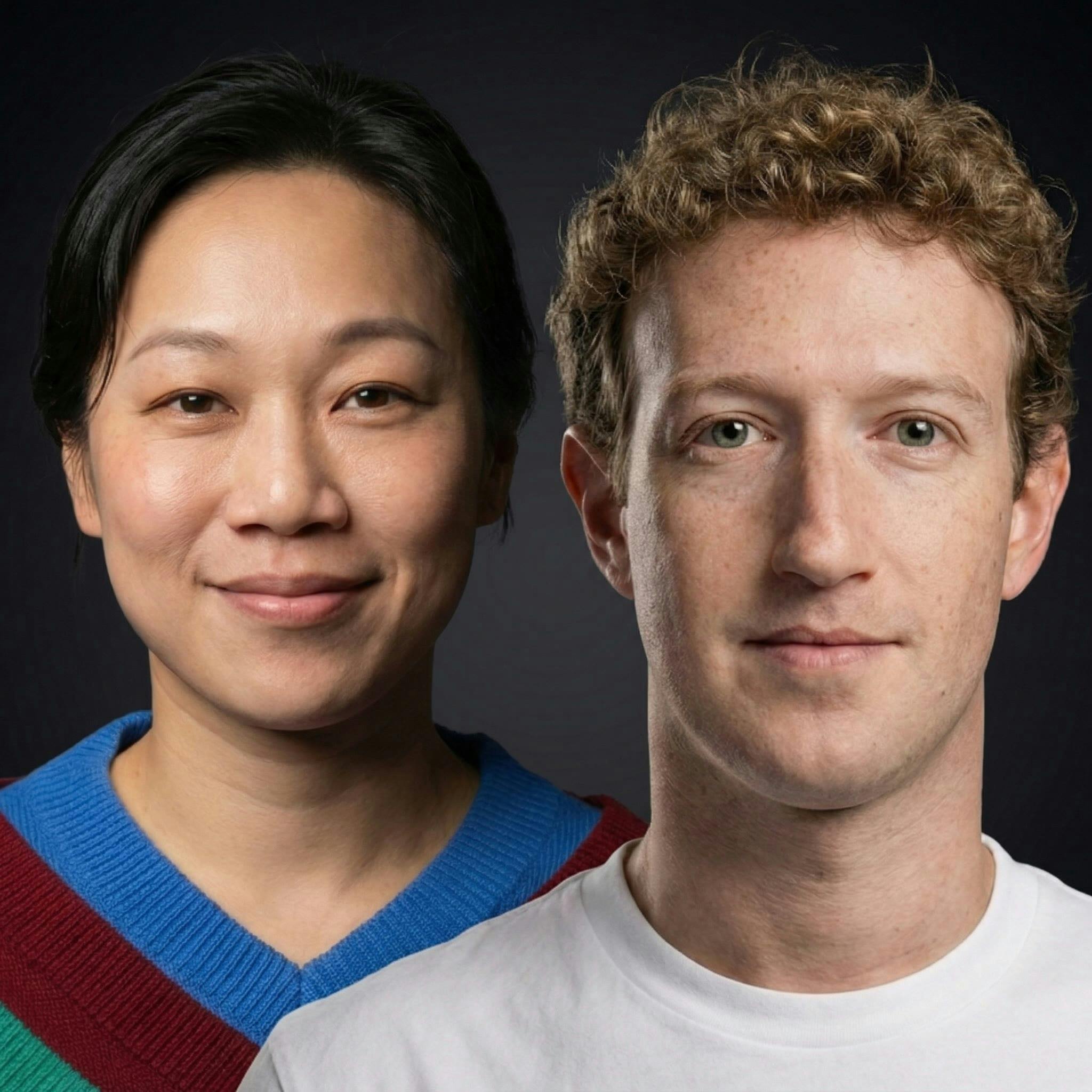
The endgame for CZI's work is hyper-personalized, "N of one" medicine. Instead of the current empirical approach (e.g., trying different antidepressants for months), AI models will simulate an individual's unique biology to predict which specific therapy will work, eliminating guesswork and patient suffering.
Eroom's Law (Moore's Law reversed) shows rising R&D costs without better success rates. A key culprit may be the obsession with mechanistic understanding. AI 'black box' models, which prioritize predictive results over explainability, could break this expensive bottleneck and accelerate the discovery of effective treatments.
While AI can accelerate the ideation phase of drug discovery, the primary bottleneck remains the slow, expensive, and human-dependent clinical trial process. We are already "drowning in good ideas," so generating more with AI doesn't solve the fundamental constraint of testing them.
The future of AI in drug discovery is shifting from merely speeding up existing processes to inventing novel therapeutics from scratch. The paradigm will move toward AI-designed drugs validated with minimal wet lab reliance, changing the key question from "How fast can AI help?" to "What can AI create?"
Despite AI's power, 90% of drugs fail in clinical trials. John Jumper argues the bottleneck isn't finding molecules that target proteins, but our fundamental lack of understanding of disease causality, like with Alzheimer's, which is a biology problem, not a technology one.
The process of testing drugs in humans—clinical development—is a massive, under-studied bottleneck, accounting for 70% of drug development costs. Despite its importance, there is surprisingly little public knowledge, academic research, or even basic documentation on how to improve this crucial stage.
AI will create jobs in unexpected places. As AI accelerates the discovery of new drugs and medical treatments, the bottleneck will shift to human-centric validation. This will lead to significant job growth in the biomedical sector, particularly in roles related to managing and conducting clinical trials.
Despite major scientific advances, the key metrics of drug R&D—a ~13-year timeline, 90-95% clinical failure rate, and billion-dollar costs—have remained unchanged for two decades. This profound lack of productivity improvement creates the urgent need for a systematic, AI-driven overhaul.
The immediate goal for AI in drug design is finding initial "hits" for difficult targets. The true endgame, however, is to train models on manufacturability data—like solubility and stability—so they can generate molecules that are already optimized, drastically compressing the development timeline.