Despite initial hype in oncology where business models struggled, cell therapy is finding a major new application in treating autoimmune diseases. By resetting the immune system, it can offer functional cures for debilitating conditions—a powerful and unexpected pivot for the technology platform.
Related Insights
The focus in advanced therapies has shifted dramatically. While earlier years were about proving clinical and technological efficacy, the current risk-averse funding climate has forced the sector to prioritize commercial viability, scalability, and the industrialization of manufacturing processes to ensure long-term sustainability.
Despite exciting early efficacy data for in vivo CAR-T therapies, the modality's future hinges on the critical unanswered question of durability. How long the therapeutic effects last, for which there is little data, will ultimately determine its clinical viability and applications in cancer versus autoimmune diseases.
The current boom in immunology and autoimmune (I&I) therapeutics is not a separate phenomenon but a direct consequence of capital and knowledge from immuno-oncology. Many of the same biological pathways are being targeted, simply modulated down (for autoimmune) instead of up (for cancer), allowing for rapid therapeutic advancement and platform reuse.
Early data from an in vivo CAR-T therapy suggests a paradigm shift is possible. By engineering T-cells directly inside the patient with a simple infusion, this approach could eliminate the need for leukapheresis and external manufacturing, completely disrupting the current cell therapy model.
While many cell therapies rely on complex genetic engineering with viral vectors, Adaptin Bio manipulates patient T-cells without it. This simpler, non-viral process is a strategic choice to reduce costs, speed up manufacturing, and make the therapy accessible to a broader patient population.
Despite significant progress in managing symptoms for autoimmune conditions, very few treatments fundamentally alter the disease's course. The major unmet needs and investment opportunities lie in therapies that can induce remission or target common underlying pathologies like fibrosis, moving beyond mere symptom relief.
Beyond its lead product Orca T for matched donors, the company is building a broader platform. Its Orca Q program addresses mismatched donors, expanding the patient pool. Furthermore, collaborations to combine Orca T with allogeneic CAR-T therapies position the technology as a foundational solution for overcoming key hurdles in the wider cell therapy field.
Rather than expecting cell therapies (CAR-T, TIL) to eradicate every cancer cell, Dr. Radvanyi reframes them as powerful adjuvants. Their role is to inflict initial damage, kill tumor cells, and release antigens, creating an opportunity to prime a broader, secondary immune response with other modalities like vaccines or checkpoint inhibitors.
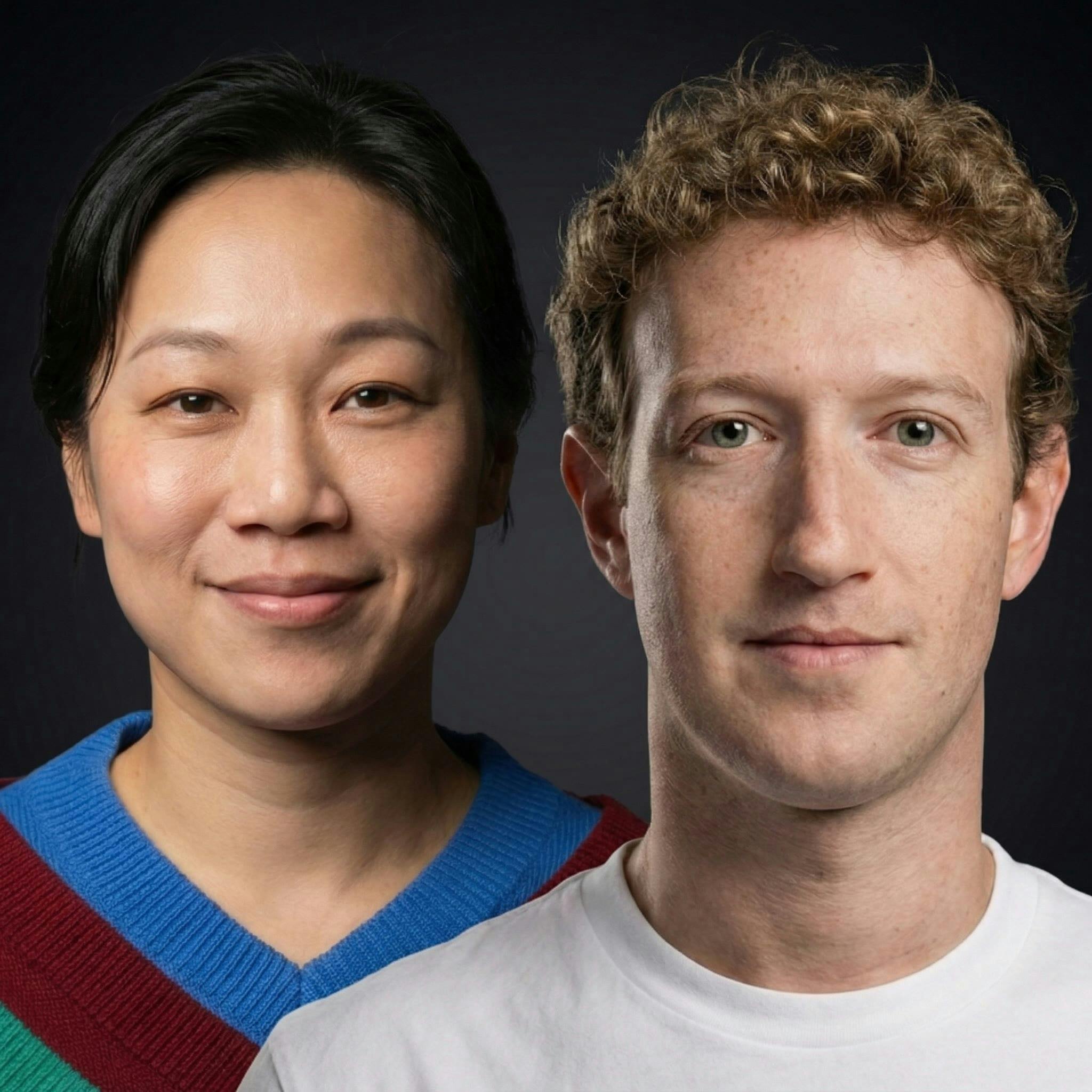
The immune system is the initial target for CZI's virtual cell modeling because of its strategic importance. As a mobile system that touches every part of the body, understanding and engineering it offers a powerful lever to address a vast range of conditions, including cancer and autoimmune diseases.
The T-cell delivery system is versatile. It can carry T-cell engagers for cancer, but also antibodies for Alzheimer's or oligonucleotides. By using different T-cell types (like regulatory T-cells), it can also be used to reduce inflammation, expanding its applicability beyond oncology.