Surprisingly, patients with high-risk cytogenetics, a typically poor prognostic factor in multiple myeloma, were equally represented in both the long-term remission group and the group that progressed after Siltacel treatment. This suggests CAR-T therapy may overcome traditional risk stratification.
Related Insights
In the Cartitude 1 trial, the strongest predictor of long-term remission with Siltacel was a lower burden of disease (measured by bone marrow percentage and soluble BCMA levels), rather than the number of prior treatments. This implies using CAR-T therapy earlier in the disease course is more effective.
Data from J&J's Majestic 3 trial suggests its off-the-shelf bispecific combination could rival the efficacy of its own blockbuster CAR-T, Carvykti. This sets up an internal competition where a more accessible therapy could challenge a complex, personalized one in earlier lines of treatment.
A common multiple myeloma treatment, autologous stem cell transplant, causes a significant decrease in beneficial, butyrate-producing gut bacteria. This treatment-induced change is directly associated with inferior progression-free survival, revealing a paradoxical negative effect of a standard therapy.
Despite exciting early efficacy data for in vivo CAR-T therapies, the modality's future hinges on the critical unanswered question of durability. How long the therapeutic effects last, for which there is little data, will ultimately determine its clinical viability and applications in cancer versus autoimmune diseases.
The efficacy of Siltacel stems from a powerful initial expansion that eliminates cancer upfront. The CAR-T cells are often undetectable beyond six months, indicating their curative potential comes from an overwhelming initial response rather than persistent, long-term immune policing of the disease.
Using a BCMA bispecific antibody first can exhaust a patient's T-cells or cause tumors to lose the BCMA target, rendering a subsequent BCMA-targeted CAR-T therapy ineffective. The optimal sequence is CAR-T first, which preserves T-cell function and BCMA expression, leaving bispecifics as a viable later-line option.
The term "functional cure" is misleading and hinders progress. With one-third of heavily pretreated patients in the Cartitude 1 trial remaining disease-free for five years without maintenance, the data supports the classical definition of a "cure" used in other cancers. This semantic shift is crucial for advancing the field.
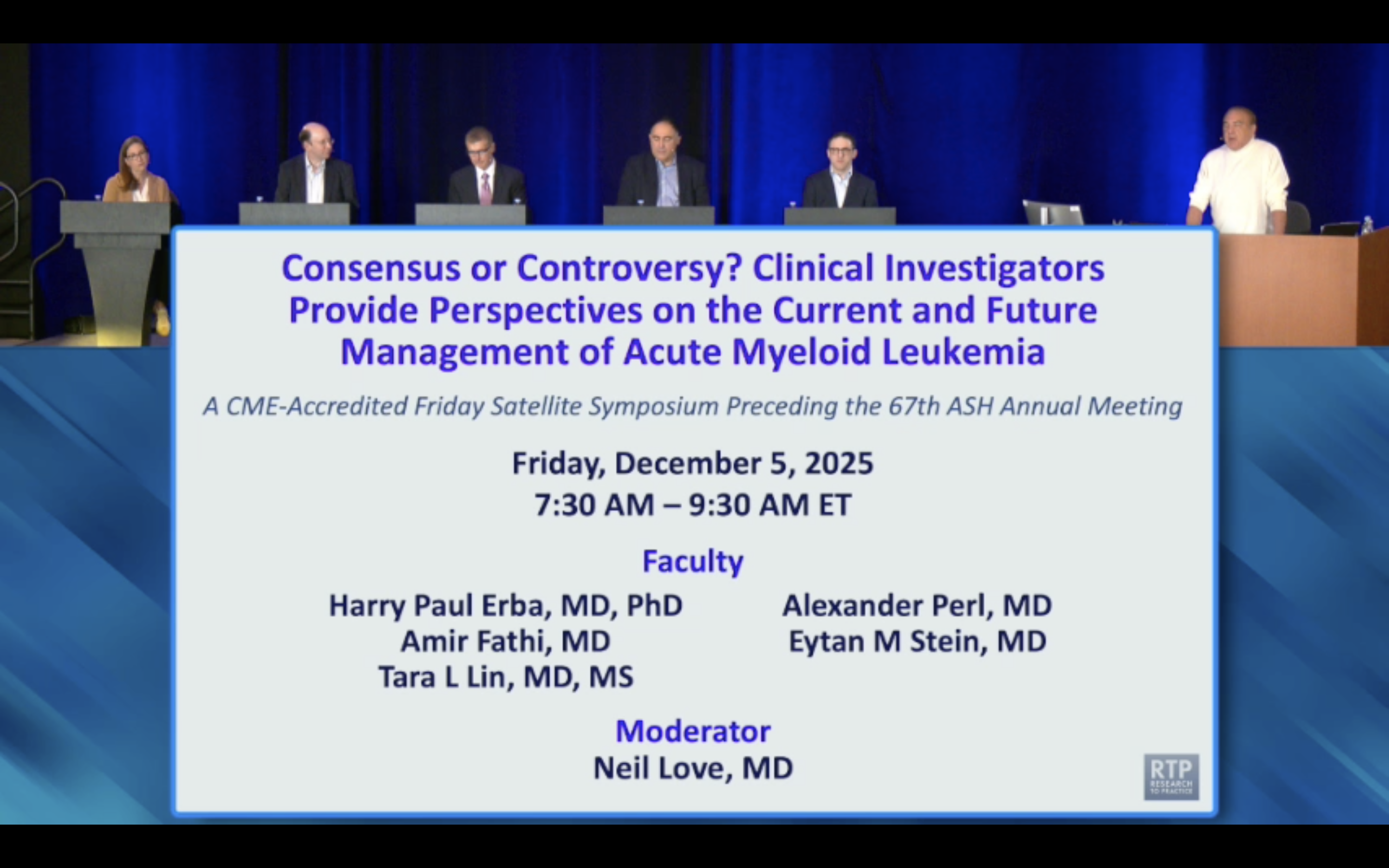
TP53-mutated AML carries an extremely poor prognosis, significantly worse than other adverse-risk subtypes. When TP53 patients are excluded from analyses, the survival gap between the remaining adverse-risk and intermediate-risk patients narrows considerably, clarifying risk stratification.
The success of CAR-T therapy hinges on the quality of the patient's own lymphocytes. Procuring T-cells earlier in the disease course, before they become exhausted from numerous prior therapies, results in a higher proportion of naive T-cells, leading to better CAR-T cell manufacturing and clinical outcomes.
A key breakthrough in Colonia Therapeutics' early data is achieving profound CAR-T cell expansion without lymphodepleting chemotherapy. This dramatically improves the safety profile and patient experience, potentially moving CAR-T therapy from major academic centers to more accessible community oncology settings, thereby "democratizing" the treatment.