The field of multiple myeloma has transformed from having few treatments to an abundance of effective drugs. The primary clinical challenge is no longer finding a therapy that works, but rather determining the optimal sequence and combination of available options, highlighting a unique form of market maturity.
Related Insights
The focus in advanced therapies has shifted dramatically. While earlier years were about proving clinical and technological efficacy, the current risk-averse funding climate has forced the sector to prioritize commercial viability, scalability, and the industrialization of manufacturing processes to ensure long-term sustainability.
An expert argues the path to curing metastatic cancer may mirror pediatric ALL's history: combining all highly active drugs upfront. Instead of sequencing treatments after failure, the focus should be on powerful initial regimens that eradicate cancer, even if it means higher initial toxicity.
When a highly effective therapy like EV Pembro was approved for 'cisplatin ineligible' patients, the definition of 'ineligible' became very elastic in practice. This demonstrates that when a new treatment is seen as transformative, clinicians find ways to qualify patients, putting pressure on established guidelines.
The future of medicine isn't about finding a single 'best' modality like CAR-T or gene therapy. Instead, it's about strategic convergence, choosing the right tool—be it a bispecific, ADC, or another biologic—based on the patient's specific disease stage and urgency of treatment.
Despite strong single-agent trial results, experts believe the field is shifting away from continuous monotherapy. The most significant future impact for pirtobrutinib will likely be as a backbone of fixed-duration combination therapies with drugs like venetoclax, aiming for deeper remissions without indefinite treatment.
The effectiveness of modern daratumab-based therapies has significantly improved patient outcomes. This positive development paradoxically made previous staging systems, founded in eras with less effective treatments, unable to accurately identify the highest-risk patients, necessitating the creation of a new prognostic model for the current era.
Rather than moving through distinct lines of therapy, a future strategy could involve an "ADC switch." When a patient progresses on an ADC-IO combination, the IO backbone would remain while the ADC is swapped for one with a different, non-cross-resistant mechanism, adapting the treatment in real-time.
Orca Bio's initial trials focused on younger patients who can withstand intense chemotherapy. Now, they are strategically expanding their addressable market by demonstrating Orca T's effectiveness with reduced-intensity conditioning. This makes the curative therapy safer and accessible to a larger population of older or frailer patients.
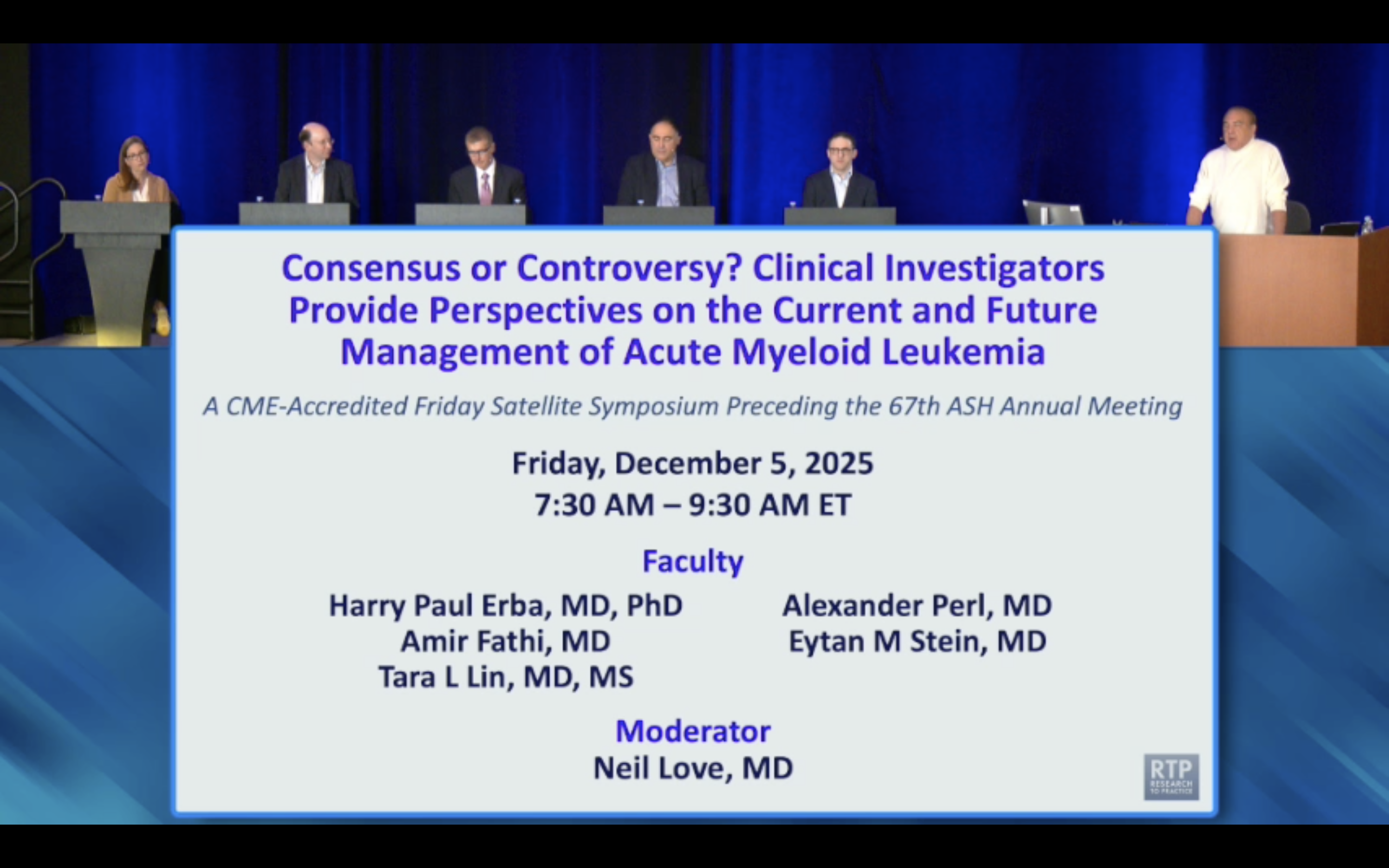
Traditional age cutoffs for AML therapy are becoming obsolete. A comprehensive fitness assessment, not just chronological age, should guide treatment, as some guidelines now classify patients as young as 55 as "older adults," a surprising shift for many clinicians.
The PSMA edition trial's fixed six-cycle Lutetium regimen, designed nearly a decade ago, is now seen as suboptimal. This illustrates how the long duration of clinical trials means their design may not reflect the latest scientific understanding (e.g., adaptive dosing) by the time results are published and debated.