The treatment backbone for Ph+ ALL is shifting away from intensive chemotherapy like hyper-CVAD. Chemotherapy-free regimens combining blinatumomab with a TKI (preferably ponatinib) are becoming the new standard, showing outcomes that are at least as good as, and likely better than, traditional chemotherapy.
Related Insights
Non-covalent BTK inhibitors like pirtobrutinib are currently approved for use after covalent BTK inhibitors fail. Moving them to the frontline setting, as studied in BRUIN-313, disrupts the established treatment pathway and creates uncertainty for managing relapsed disease, as the standard 'next step' is removed.
The FLAG-IDA plus venetoclax regimen achieves very high MRD-negative remission rates. However, its similar efficacy in both frontline and first salvage settings suggests it might be more strategically deployed as a salvage therapy, avoiding its high toxicity in all patients upfront.
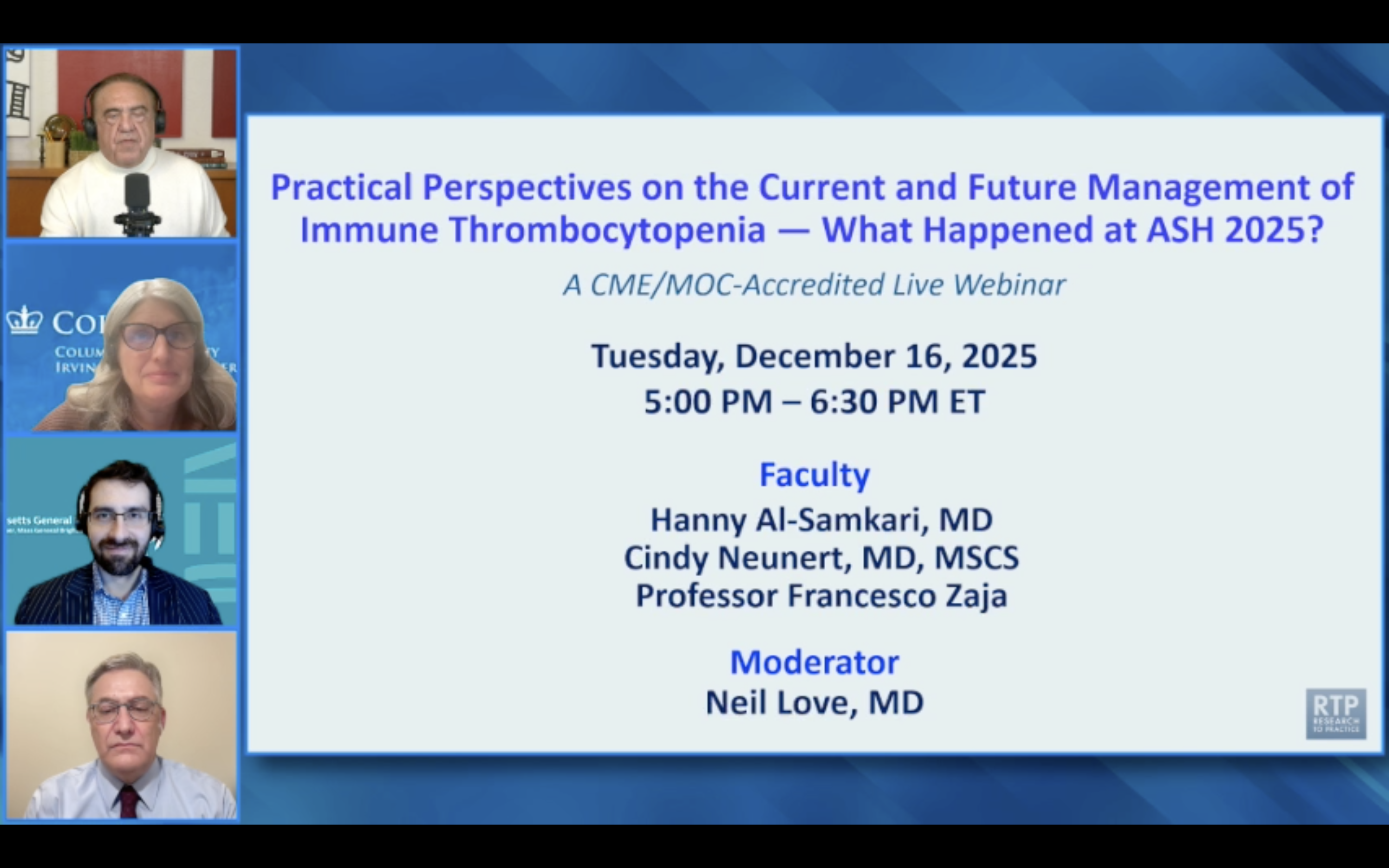
The treatment paradigm for ITP is shifting towards early combination therapy. Recent clinical trials are investigating augmented first- and second-line regimens, such as combining dexamethasone with rituximab or romiplostim, to achieve more durable, treatment-free responses than monotherapy.
An expert argues the path to curing metastatic cancer may mirror pediatric ALL's history: combining all highly active drugs upfront. Instead of sequencing treatments after failure, the focus should be on powerful initial regimens that eradicate cancer, even if it means higher initial toxicity.
The development of agents targeting specific mutations like CALR and JAK2V617F marks a move away from the "one size fits all" JAK inhibitor approach. This enables a more personalized, molecularly-driven treatment strategy that was previously not possible for MPN patients.
Early data from the CLL 314 study shows a progression-free survival benefit for pirtobrutinib over ibrutinib in frontline CLL patients. This finding suggests a potential future shift where non-covalent BTK inhibitors could become the initial standard of care.
Despite the high likelihood (75%) of a T315I mutation at relapse on first or second-generation TKIs, testing is not critical for the immediate treatment decision. The most potent TKI, ponatinib, would be the next line of therapy regardless of the mutation status, making the test more of a confirmation than a decision driver.
Despite strong single-agent trial results, experts believe the field is shifting away from continuous monotherapy. The most significant future impact for pirtobrutinib will likely be as a backbone of fixed-duration combination therapies with drugs like venetoclax, aiming for deeper remissions without indefinite treatment.
While blinatumomab-TKI combinations avoid systemic chemotherapy toxicity, they are associated with higher rates of central nervous system (CNS) relapses. This necessitates an increased number of intrathecal chemotherapy doses to prevent CNS disease, a critical nuance for managing this 'simpler' approach.
A key nuance in managing ponatinib for Ph+ ALL is a response-adapted dosing strategy. Patients are typically started at a 30mg dose, which is then reduced to 15mg once a good minimal residual disease (MRD) response is achieved. This approach aims to maintain efficacy while mitigating long-term toxicity.